This post is the second in a multi-part series, covering how GiveWell works and what we fund. The first post, on cost-effectiveness, is here. Through these posts, we hope to give a better understanding of our research and decision-making.
Looking forward, not just backward
When we consider recommending funding, we don’t just want to know whether a program has generally been cost-effective in the past—we want to know how additional funding would be used.
People sometimes think of GiveWell as recommending entire programs or organizations. This was more accurate in GiveWell’s early days, but now we tend to narrow in on specific opportunities. Rather than asking whether it is cost-effective to deliver long-lasting insecticide-treated nets in general, we ask more specific questions, such as whether it is cost-effective to fund net distributions in 2023 in the Nigerian states of Benue, Plateau, and Zamfara, given the local burden of malaria and the costs of delivering nets in those states.
Geographic factors affecting cost-effectiveness
The same program can vary widely in cost-effectiveness across locations. The burden of a disease in a particular place is often a key factor in determining overall cost-effectiveness. All else equal, it’s much more impactful to deliver vitamin A supplements in areas with high rates of vitamin A deficiency than in areas where almost everyone consumes sufficient vitamin A as part of their diet. Similarly, one of our top charities, New Incentives, has chosen to operate in northern Nigeria largely because relatively low baseline vaccination rates mean its work is especially impactful there.[1]
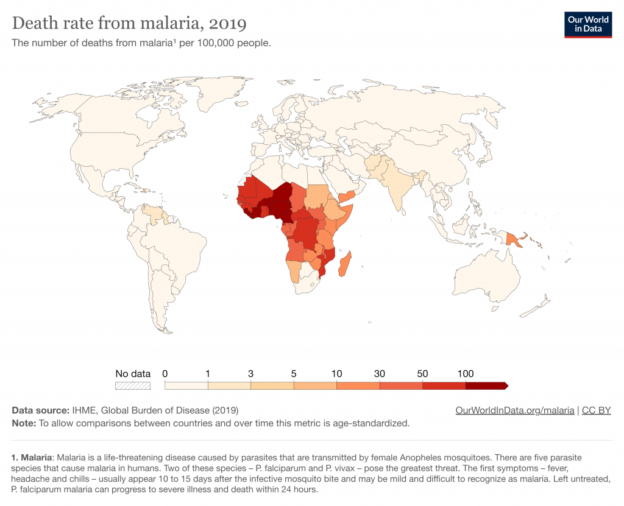
As another example, we estimate it costs roughly the same amount for the Against Malaria Foundation to deliver an insecticide-treated net in Chad as it does in Guinea (about $4 in both locations). But, we estimate that malaria-attributable deaths of young children in the absence of nets would be roughly 5 times higher in Guinea than in Chad (roughly 8.8 deaths per 1,000 per year versus roughly 1.7 per 1,000), which leads AMF’s program to be much more cost-effective in Guinea. Overall, we estimate that AMF’s program is around 27x cash in Guinea and around 5x cash in Chad.[2]
This map from Our World in Data gives a sense of how deaths from malaria vary worldwide.[3]
Because cost-effectiveness varies with geography, we ask questions specific to the countries or regions where a program
Givewell Blog | http://feeds.feedburner.com/TheGivewellBlog